Supporting physical activity through co-production in people with severe mental ill health.
THE PROBLEM
People with severe mental ill health die on average 15-20 years earlier than those in the general population and the main cause of these early deaths is due to preventable physical diseases such as cardiovascular disease and diabetes. One of the ways that people can improve their physical health and reduce their chances of developing cardiovascular disease or diabetes is by taking part in physical activity.
OUR PROJECT
SPACES is a research project whose aim is to develop an intervention to help people with severe mental ill health to become more active. The project is a collaboration between researchers and people with lived experience of severe mental ill health. Researchers from the University of York, Leeds, Sheffield, Sheffield Hallam, Northumbria and King’s College London along with Sheffield Health and Social Care NHS have worked with people with lived experience to explore the barriers and facilitators to people with severe mental ill health taking part in physical activity. Based on the findings from these workshops the team are preparing a funding application to develop an intervention to help people with severe mental ill health become more active.
CO-PRODUCTION IN ACTION




Designing the SPACES intervention
In 2021, having successfully received funding from NIHR Programme Research Grant, the SPACES team began developing an intervention aimed at improving levels of physical activity and reducing levels of sedentary behaviour in people living with a severe mental illness.
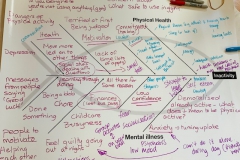
The SPACES team gathered information from multiple sources to find out about current physical activity levels of people with severe mental illness, the barriers and motivators they experience when taking part in physical activity and the components used in previous effective physical activity interventions. This involved conducting:
• The Physical Activity Survey which received (529) responses from people living with a severe mental illness
• A series of focus groups with people living with a severe mental illness, people who care for those living with severe mental illness and health professionals who have experience of working either in physical activity or with people who have a severe mental illness
• A systematic review of published research literature reporting the outcomes of previous physical activity interventions for people with severe mental illness
The information gathered from these sources was shared with our ‘Consensus Group’ made up of stakeholders (people with severe mental illness, carers and health professionals who support people with severe mental illness) who worked alongside the research team to develop the components of the SPACES intervention and review the final design and accompanying materials.
The SPACES intervention is an 18-week physical activity programme that features:
- Weekly group sessions, led by two trained Physical Activity Coordinators, with up to 60 minutes of physical activity, 30 minutes for a themed discussion on topics surrounding physical activity, and 30 minutes for socialising and addressing any queries.
- 1-to-1 support between Physical Activity Coordinator and participant at regular intervals throughout the intervention, including long form consultations (45 to 60 minutes) and brief check-ins (15 to 30 minutes).
- Weekly session attendance prompts.
- Peer support from those taking part in the intervention (e.g. participants may choose to create a WhatsApp group to keep in touch outside of weekly sessions).
- Additional optional resources such as a participant handbook and a pedometer.
What is happening now in the SPACES research project?
Now that the SPACES physical activity intervention has been designed, the next step in the SPACES research project is to trial our intervention on a small scale, to find out if it is acceptable to those who take part in it and feasible to trial on a much larger scale. This type of trial is sometimes referred to as a feasibility trial. We will work with different NHS trusts across England to deliver this intervention within the trust’s local area.
People living with a severe mental illness who are interested in increasing their levels of physical activity and are eligible to take part will be invited to participate by staff at their local NHS trust such as their care coordinator.
Participants will be randomised to either continue their treatment as usual or to take part in the SPACES intervention alongside their usual treatment. Both groups of participant’s are really important in this trial as this allows researchers to compare the experiences of those taking part in the intervention and those who did not. Making this comparison is crucial because at the moment, nobody knows what difference the SPACES physical activity intervention will make (if any!).
Researchers will measure all participant’s physical activity levels at the beginning, middle and end of the trial. At each of these time points, participants will also be asked to complete questionnaires about things like their physical and mental health and quality of life.
At the end of the trial, some of the participants who took part in the SPACES intervention will be invited to a short interview to find out about their experiences of the intervention, as will some of the Physical Activity Coordinators who delivered it.
Using the information collected from the physical activity measures and questionnaires, researchers will be able to investigate if there were any differences between the group of participants who took part in the intervention and those did not. Also, using the feedback collected from the interviews, researchers will be able to investigate how well the intervention was received and if any changes need to be made before beginning a larger scale trial.









